Promotion
Use code FALL24 for 20% off sitewide!
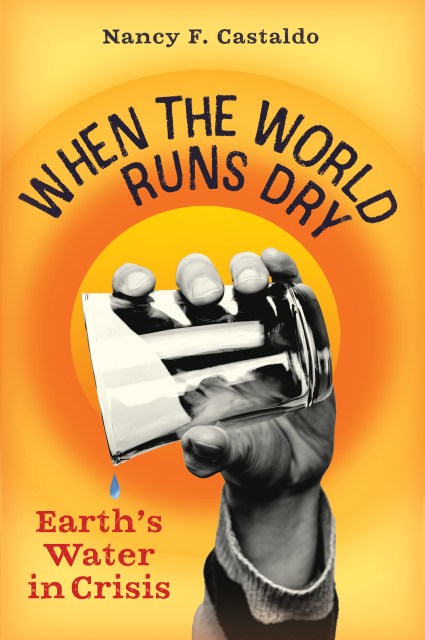
When the World Runs Dry
Earth's Water in Crisis
Contributors
Formats and Prices
Price
$16.95Price
$22.95 CADFormat
Format:
- Hardcover $16.95 $22.95 CAD
- ebook $11.99 $15.99 CAD
- Audiobook Download (Unabridged) $18.99
This item is a preorder. Your payment method will be charged immediately, and the product is expected to ship on or around January 18, 2022. This date is subject to change due to shipping delays beyond our control.
Also available from:
A riveting account of the worldwide water crisis–and what kids can do about it–from an award-winning science writer.
What would you do if you turned on the faucet one day and nothing happened? What if you learned the water in your home was harmful to drink? Water is essential for life on this planet, but not every community has the safe, clean water it needs. In When the World Runs Dry, award-winning science writer Nancy Castaldo takes readers from Flint, Michigan, and Newark, New Jersey, to Iran and Cape Town, South Africa, to explore the various ways in which water around the world is in danger, why we must act now, and why you’re never too young to make a difference.
Topics include: Lead and water infrastructure problems, pollution, fracking contamination, harmful algal blooms, water supply issues, rising sea levels, and potential solutions.
-
A Skipping Stones Award Honoree
Short-listed for the Green Earth Book Award
A Junior Library Guild Selection
"This refreshingly (no pun intended) readable and engrossing book on the state of the world's water supply is an important read." --Youth Services Review, 5-star review
"This is the book to read if you want to go from depressed to fired-up and ready for action." --Audubon
"The narrative balances wide-ranging information with accessible prose . . . [an] invaluable tome that underscores an imperative crisis." --Publishers Weekly
"Impeccably researched and sourced . . . This book holds substantial value as a classroom text." --Booklist
- On Sale
- Jan 18, 2022
- Page Count
- 208 pages
- Publisher
- Algonquin Young Readers
- ISBN-13
- 9781616209711
Newsletter Signup
By clicking ‘Sign Up,’ I acknowledge that I have read and agree to Hachette Book Group’s Privacy Policy and Terms of Use