Promotion
Use code MOM24 for 20% off site wide + free shipping over $45
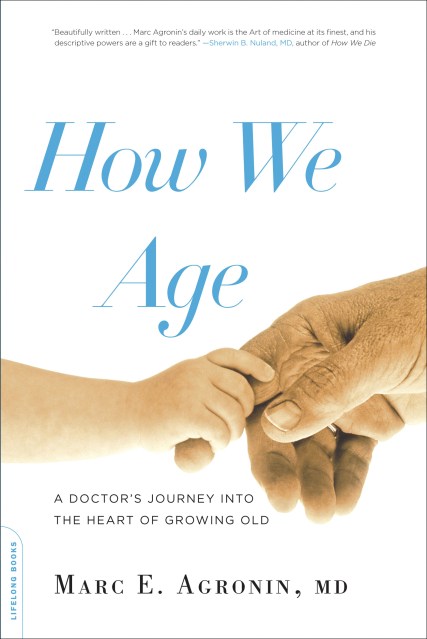
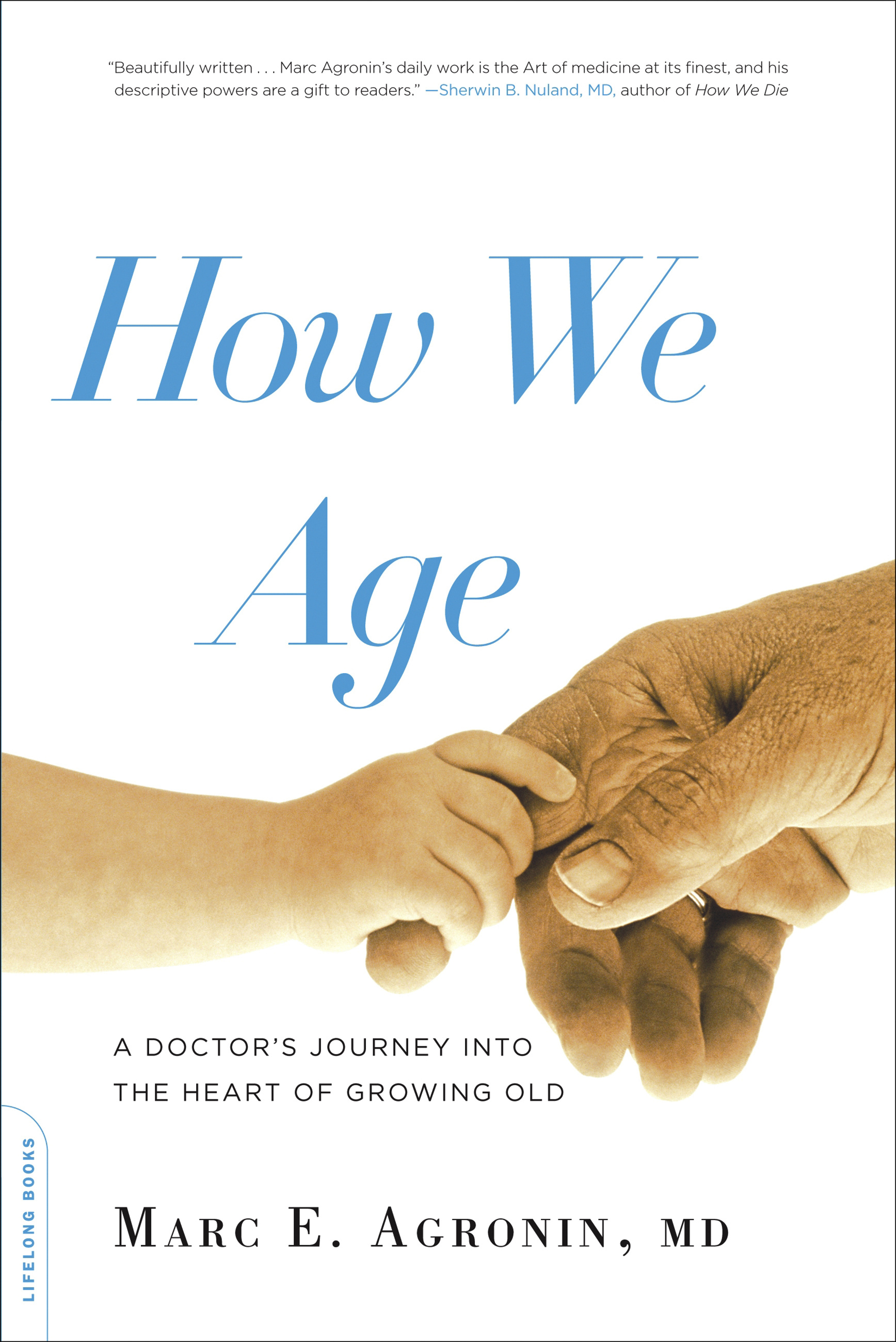
How We Age
A Doctor's Journey into the Heart of Growing Old
Contributors
Formats and Prices
Price
$21.99Price
$28.99 CADFormat
Format:
- Trade Paperback $21.99 $28.99 CAD
- ebook $9.99 $12.99 CAD
This item is a preorder. Your payment method will be charged immediately, and the product is expected to ship on or around March 6, 2012. This date is subject to change due to shipping delays beyond our control.
Also available from:
Genre:
- On Sale
- Mar 6, 2012
- Page Count
- 320 pages
- Publisher
- Da Capo Lifelong Books
- ISBN-13
- 9780738215587
Newsletter Signup
By clicking ‘Sign Up,’ I acknowledge that I have read and agree to Hachette Book Group’s Privacy Policy and Terms of Use