Promotion
Use code MOM24 for 20% off site wide + free shipping over $45
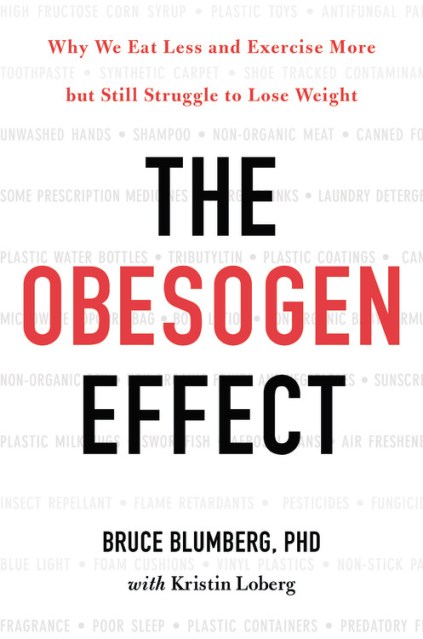
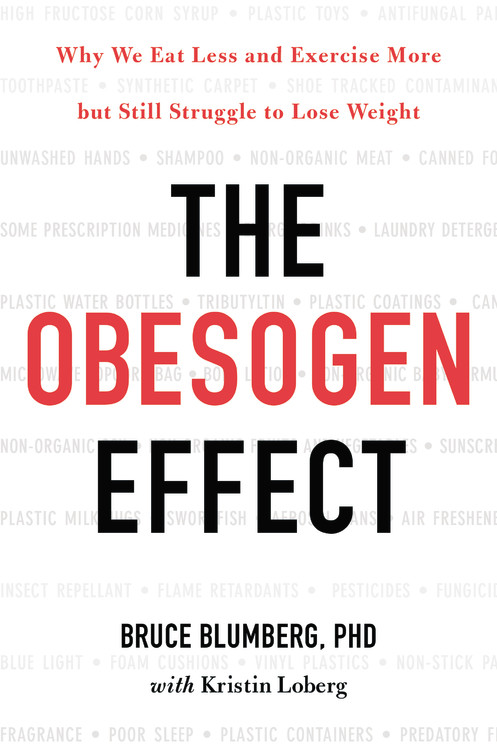
The Obesogen Effect
Why We Eat Less and Exercise More but Still Struggle to Lose Weight
Contributors
With Kristin Loberg
Formats and Prices
Price
$37.00Price
$47.00 CADFormat
Format:
- Hardcover $37.00 $47.00 CAD
- ebook $14.99 $19.99 CAD
- Audiobook Download (Unabridged)
This item is a preorder. Your payment method will be charged immediately, and the product is expected to ship on or around March 20, 2018. This date is subject to change due to shipping delays beyond our control.
Also available from:
Being overweight is not just the result of too many cheeseburgers or not enough exercise. According to leading-edge science, a new group of silent saboteurs in our daily lives is contributing greatly to our obesity epidemic: obesogens. These weight-inducing offenders, most of which are chemicals, disrupt our hormonal systems, altering how we create and store fat, and changing how we respond to dietary choices and caloric intake. Because they are largely unregulated, obesogens lurk all around us-in food, furniture, plastic products such as water bottles and food storage containers, and other surprising exposure points. Even worse: research has shown that the effects of some obesogens can be passed on to future generations by irreversibly interfering with the expression of our genes. The good news is we can protect ourselves by becoming more informed consumers.
In The Obesogen Effect, Dr. Bruce Blumberg explains how obesogens work, where they are found, and how we can minimize their effects. Dr. Blumberg offers a highly practical three-step solution for reducing exposures. He explains why one size does not fit all in a weight loss program, what harmful additives are in our household goods, and how we should shop for obesogen-free items we use every day-from vegetables and meats to canned soup as well as household cleaners, air fresheners, and personal care products. The Obesogen Effect, is an urgent call to action to protect your body, clean up your life, and set a straight course for better health.
Genre:
- On Sale
- Mar 20, 2018
- Page Count
- 320 pages
- Publisher
- Grand Central Life & Style
- ISBN-13
- 9781478970644
Newsletter Signup
By clicking ‘Sign Up,’ I acknowledge that I have read and agree to Hachette Book Group’s Privacy Policy and Terms of Use