Promotion
Use code MOM24 for 20% off site wide + free shipping over $45
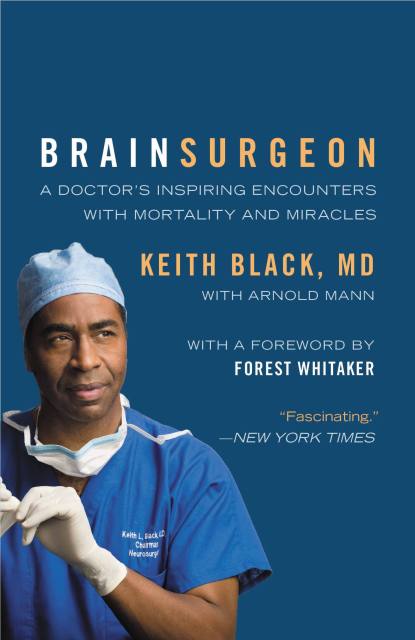
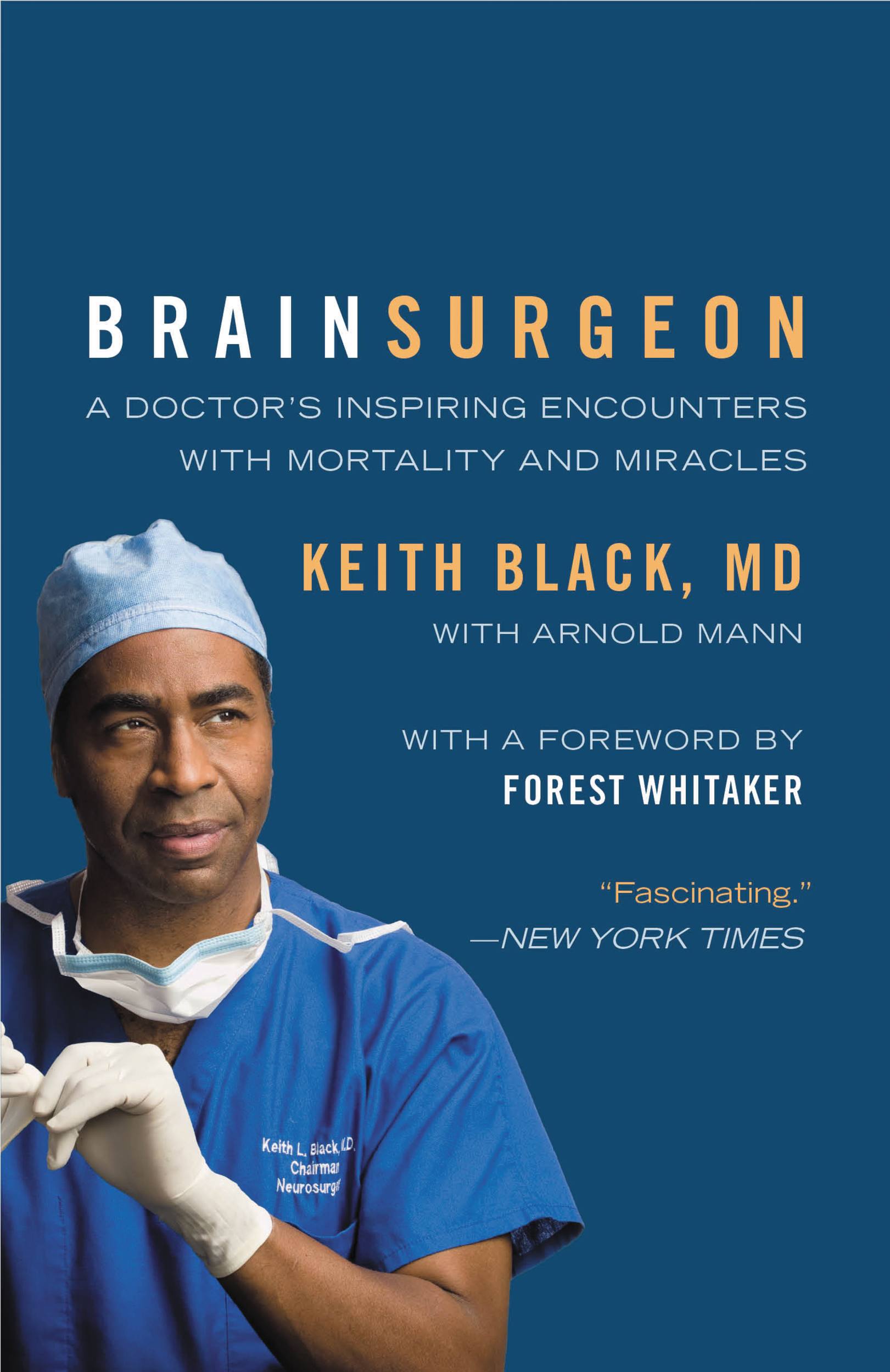
Brain Surgeon
A Doctor's Inspiring Encounters with Mortality and Miracles
Contributors
By Arnold Mann
Formats and Prices
Price
$9.99Price
$12.99 CADFormat
Format:
- ebook $9.99 $12.99 CAD
- Trade Paperback $19.99 $25.99 CAD
This item is a preorder. Your payment method will be charged immediately, and the product is expected to ship on or around March 25, 2009. This date is subject to change due to shipping delays beyond our control.
Also available from:
Dr. Black invites readers to shadow his breathtaking journeys into the brain as he battles some of the deadliest and most feared tumors known to medical science.
Welcome to tiger country: the treacherous territory where a single wrong move by a brain surgeon can devastate-or end-a patient's life. This is the terrain world-renowned neurosurgeon Keith Black, MD, enters every day to produce virtual medical miracles. Along the way, he shares his unique insights about the inner workings of the brain, his unwavering optimism for the future of medicine, and the extraordinary stories of his patients-from ministers and rock stars to wealthy entrepreneurs and uninsured students-whom he celebrates as the real heroes.
Brain Surgeon offers a window into one man's remarkable mind, revealing the anatomy of the unflinching confidence of this master surgeon, whose personal journey brought him from life as a young African-American boy growing up in the civil rights era South to the elite world of neurosurgery. Through Dr. Black's white-knuckle descriptions of some of the most astonishing medical procedures performed today, he reveals the beauty and marvel of the human brain and the strength and heroism of his patients who refuse to see themselves as victims. Ultimately, Brain Surgeon is an inspiring story of the struggle to overcome odds-whether as a man, a doctor, or a patient.
Praise for Brain Surgeon "An inspirational book about true heroes – readers will marvel at Keith Black's achievements both as a doctor and as a man, and will be in awe of his patients' courage and will to survive." — Denzel Washington
"A rare, behind-the-curtain look at the life of one of the most pre-eminent neurosurgeons in the world." — Sanjay Gupta, MD, Chief Medical Correspondent, CNN
Welcome to tiger country: the treacherous territory where a single wrong move by a brain surgeon can devastate-or end-a patient's life. This is the terrain world-renowned neurosurgeon Keith Black, MD, enters every day to produce virtual medical miracles. Along the way, he shares his unique insights about the inner workings of the brain, his unwavering optimism for the future of medicine, and the extraordinary stories of his patients-from ministers and rock stars to wealthy entrepreneurs and uninsured students-whom he celebrates as the real heroes.
Brain Surgeon offers a window into one man's remarkable mind, revealing the anatomy of the unflinching confidence of this master surgeon, whose personal journey brought him from life as a young African-American boy growing up in the civil rights era South to the elite world of neurosurgery. Through Dr. Black's white-knuckle descriptions of some of the most astonishing medical procedures performed today, he reveals the beauty and marvel of the human brain and the strength and heroism of his patients who refuse to see themselves as victims. Ultimately, Brain Surgeon is an inspiring story of the struggle to overcome odds-whether as a man, a doctor, or a patient.
Praise for Brain Surgeon "An inspirational book about true heroes – readers will marvel at Keith Black's achievements both as a doctor and as a man, and will be in awe of his patients' courage and will to survive." — Denzel Washington
"A rare, behind-the-curtain look at the life of one of the most pre-eminent neurosurgeons in the world." — Sanjay Gupta, MD, Chief Medical Correspondent, CNN
Genre:
- On Sale
- Mar 25, 2009
- Page Count
- 240 pages
- Publisher
- Grand Central Life & Style
- ISBN-13
- 9780446544528
Newsletter Signup
By clicking ‘Sign Up,’ I acknowledge that I have read and agree to Hachette Book Group’s Privacy Policy and Terms of Use