By clicking “Accept,” you agree to the use of cookies and similar technologies on your device as set forth in our Cookie Policy and our Privacy Policy. Please note that certain cookies are essential for this website to function properly and do not require user consent to be deployed.
You Bet Your Life
From Blood Transfusions to Mass Vaccination, the Long and Risky History of Medical Innovation
Contributors
Formats and Prices
- On Sale
- Sep 21, 2021
- Page Count
- 272 pages
- Publisher
- Basic Books
- ISBN-13
- 9781541620391
Price
$28.00Price
$35.00 CADFormat
Format:
- Hardcover $28.00 $35.00 CAD
- ebook $14.99 $19.99 CAD
- Audiobook Download (Unabridged) $24.99
- Trade Paperback $19.99 $25.99 CAD
This item is a preorder. Your payment method will be charged immediately, and the product is expected to ship on or around September 21, 2021. This date is subject to change due to shipping delays beyond our control.
Buy from Other Retailers:
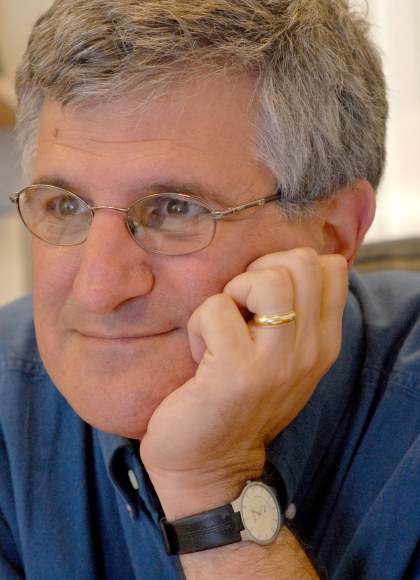
Every medical decision—whether to have chemotherapy, an X-ray, or surgery—is a risk, no matter which way you choose. In You Bet Your Life, physician Paul A. Offit argues that, from the first blood transfusions four hundred years ago to the hunt for a COVID-19 vaccine, risk has been essential to the discovery of new treatments. More importantly, understanding the risks is crucial to whether, as a society or as individuals, we accept them.
Told in Offit’s vigorous and rigorous style, You Bet Your Life is an entertaining history of medicine. But it also lays bare the tortured relationships between intellectual breakthroughs, political realities, and human foibles. Our pandemic year has shown us, with its debates over lockdowns, masks, and vaccines, how easy it is to get everything wrong. You Bet Your Life is an essential read for getting the future a bit more right.
Genre:
-
“Offit is a good storyteller, and he has some terrific stories to tell.”Cass R. Sunstein, The New York Times Book Review
-
“Dr. Offit, a pediatrician, vaccine expert and prolific author, is exquisitely attuned to the burden shouldered by the earliest recipients of medical treatments and technologies.”David A. Shaywitz, Wall Street Journal
-
“In You Bet Your Life, Offit elucidates, using compelling case studies, how we come to know what we know in science and medicine: through a mix of imagination, experimentation, successes, misses and tragedies. It's a riveting story of what is possible when confidence and humility meet, and what seems inevitable when hubris dominates. Illuminating the Covid-19 pandemic and how we got to safe and effective vaccines so quickly, it is also a timeless read for anyone interested in science, ethics, discovery and how we can better prevent the next pandemic.”Chelsea Clinton, vice chair of the Clinton Foundation
-
“Riveting and filled with fascinating details…His latest book—YOU BET YOUR LIFE— couldn’t be more timely.”Nature
-
“Offit is a fluid storyteller armed with decades of knowledge, and he provides an educative…reading experience.”Kirkus
-
“The way Offit tells the story of each medical advance is fascinating...this thorough survey is as entertaining as it is informative.”Publishers Weekly
-
“A well-written and informative look at the reality of medical advancement, including poignant examples of its often-fatal repercussions.”Library Journal
-
"What makes Paul Offit so special, beyond his extraordinary talents as a physician, vaccine-developer, and children’s advocate, is his ability to bring complicated scientific subjects to life. You Bet Your Life is the latest example—a thoughtful, beautifully written account of the risks and rewards of medical technology told through the eyes of the inventors and their patients. Tragedy is an inevitable part of the process; breakthroughs come at a human cost, even those that have saved untold millions of lives. To read this elegant book is grasp these ethical complexities—with a masterful medical writer as our guide."David Oshinsky, winner of the Pulitzer Prize in History for Polio: An American Story
-
"Paul Offit is a national treasure. He has emerged from the ranks of doctors and scientists as one of the world’s most effective communicators. In You Bet Your Life he astutely tracks the development of a variety of monumental medical breakthroughs constantly reminding us that each carried with it not only predictable and unpredictable risks but terrible failures. It is a hard message that most of us, in thinking about the price of biomedical progress, do not want to hear. But post a horrific pandemic where blunders abounded and unnecessary deaths occurred at a staggering rate, we had better heed his clear message that acknowledging and managing risk, not pretending it does not exist or simply ignoring the truth, is the key to a healthier future for you, your children and their descendants."Arthur Caplan, Mitty Professor of Bioethics, NYU Grossman School of Medicine
-
"This book is exquisitely timed for a moment in which biomedicine has delivered miraculous vaccines to a public disastrously skeptical of science. In a series of vignettes including botched polio vaccines and the first death in a gene therapy treatment, Offit shows that while science must maintain its humility in the face of complexity, the public can’t afford to lose its trust in medical science despite the inevitable tragedies that occur in pursuit of progress."Arthur Allen, author of Vaccine
Newsletter Signup
By clicking ‘Sign Up,’ I acknowledge that I have read and agree to Hachette Book Group’s Privacy Policy and Terms of Use