By clicking “Accept,” you agree to the use of cookies and similar technologies on your device as set forth in our Cookie Policy and our Privacy Policy. Please note that certain cookies are essential for this website to function properly and do not require user consent to be deployed.
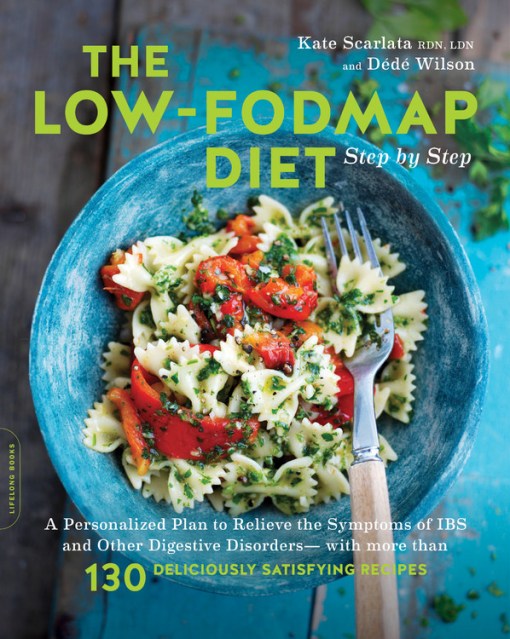
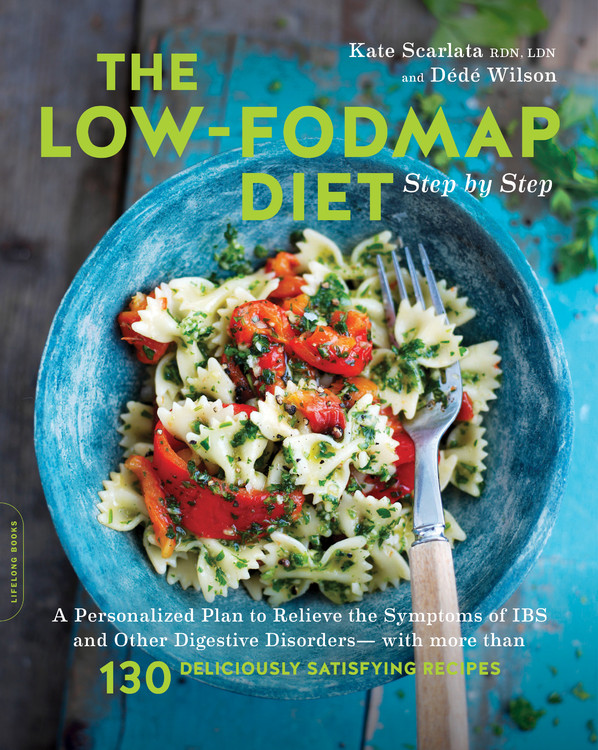
The Low-FODMAP Diet Step by Step
A Personalized Plan to Relieve the Symptoms of IBS and Other Digestive Disorders -- with More Than 130 Deliciously Satisfying Recipes
Contributors
By Dede Wilson
Formats and Prices
- On Sale
- Dec 19, 2017
- Page Count
- 384 pages
- Publisher
- Balance
- ISBN-13
- 9780738219349
Price
$23.99Price
$31.99 CADFormat
Format:
- Trade Paperback $23.99 $31.99 CAD
- ebook $15.99 $20.99 CAD
This item is a preorder. Your payment method will be charged immediately, and the product is expected to ship on or around December 19, 2017. This date is subject to change due to shipping delays beyond our control.
Buy from Other Retailers:
Do you suffer from IBS or a chronically sensitive stomach? The culprit may be your diet: many everyday foods contain FODMAPs — a group of carbohydrates that can wreak havoc on your digestive system. Digestive health specialist Kate Scarlata and expert recipe developer Dé Wilson share their clear, accessible, three-step low-FODMAP diet. Backed by the most up-to-date, sound medical advice, The Low-FODMAP Diet Step by Step walks you through:
- Identifying FODMAPs and what foods contain them
- Customizing your own gut-friendly plan to alleviate painful symptoms
- Using an elimination diet to help determine your food triggers
- Stocking your low-FODMAP pantry, with food lists and more
- Easy, delicious recipes for every meal, with specific food reintegration tips
-
"A must-read for persons seeking diet-based solutions for their gut complaints. This book is practical, easy to understand and provides a wellspring of emotional and medical inspiration."William D. Chey, MD, Nostrant Professor of Gastroenterology & Nutrition Sciences, Division of Gastroenterology, Michigan Medicine
-
"You can trust expert dietitian Kate Scarlata for accurate information, valuable insights, and practical tips about FODMAPs. The book makes the diet easy to follow--and the delicious recipes developed by Dédé Wilson help you put it into practice."Patsy Catsos, MS, RS, LD, author of The IBS Elimination Diet and Cookbook
-
"Low-FODMAP eating is a proven remedy to many suffering with chronic digestive problems, but it can be a daunting road to navigate without the right help. Enter the dream-team, Kate and Dede, top notch professionals who guide you through, step-by-step, with a clear, doable plan and excellent recipes, so you can heal and stay healthy while enjoying delicious food all along the way."Ellie Krieger, MS, RD
-
"These two experts have spun fresh, whole ingredients into culinary gold, with their all low-FODMAP recipes designed specifically for those who suffer with a sensitive gut. Let the love affair begin with homemade soups, fresh and wholesome salads and delectable baked goods. Enjoy the freedom from your IBS symptoms in this ground-breaking book, The Low-FODMAP Diet Step by Step."Suvir Saran, executive chef, cookbook author, and farmer
-
"Provid[es] easy, delicious recipes for every meal, with specific food reintegration tips. Beautifully illustrated throughout and offering thoroughly 'kitchen cook friendly' recipes that are as palate pleasing as they are appetite satisfying, The Low-FODMAP Diet Step by Step is very highly recommended for family and community library cookbook collections."Midwest Book Review
-
"A great resource with many beautiful and mouth-watering recipes...An excellent resource for dieticians."Today's Dietician
Newsletter Signup
By clicking ‘Sign Up,’ I acknowledge that I have read and agree to Hachette Book Group’s Privacy Policy and Terms of Use